What Is a DEXA Scan and Why It Matters
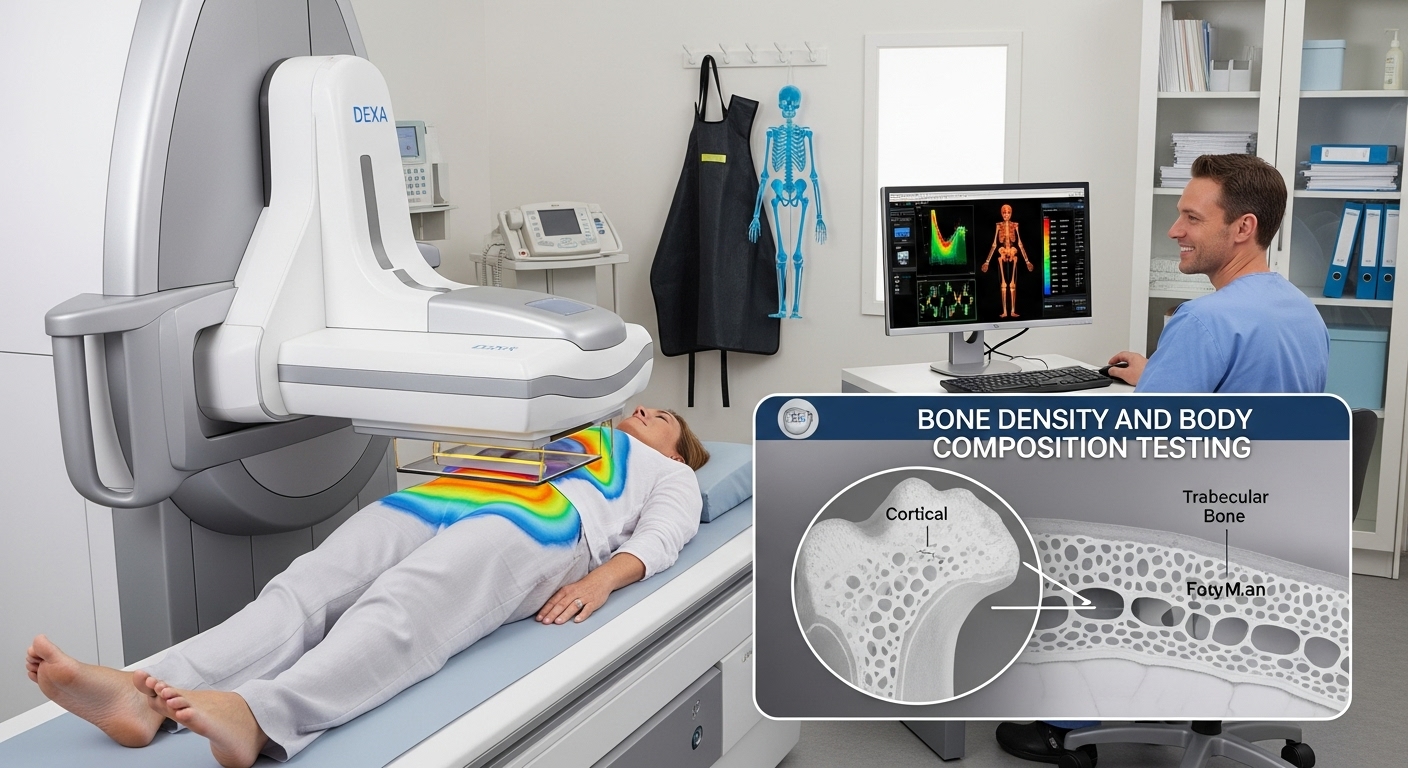
A DEXA scan represents one of the most advanced medical imaging technologies available today for assessing skeletal and body health. Healthcare professionals use this powerful diagnostic tool to measure bone mineral density and evaluate body composition with remarkable precision. Medical experts consider this imaging technique the gold standard for detecting osteoporosis and predicting fracture risk in patients. Furthermore, athletes and fitness enthusiasts increasingly rely on these scans to track their muscle mass and body fat percentages accurately.
The technology behind this scanning method uses two different x-ray beams to distinguish between bone and soft tissue effectively. Consequently, doctors can identify potential health issues before they become serious medical problems requiring extensive treatment. Many people undergo these screenings without understanding the comprehensive benefits this technology offers for long-term health monitoring and disease prevention.
The Science Behind Dual Energy X-Ray Absorptiometry Technology
Medical professionals developed this scanning technology specifically to address limitations in earlier bone density measurement techniques that proved less accurate. The system works by directing two x-ray beams with different energy levels through the body simultaneously. Moreover, these beams interact differently with various tissues, allowing sophisticated computer software to calculate precise density measurements throughout the skeletal system.
The lower energy beam gets absorbed primarily by soft tissues, while the higher energy beam penetrates deeper into bone structures. Therefore, advanced algorithms can subtract soft tissue measurements from total absorption to determine exact bone mineral content reliably. This dual-beam approach provides significantly more accurate results compared to single-energy x-ray systems used in previous decades.
Scientists have refined this technology over several decades to minimize radiation exposure while maximizing measurement accuracy for patient safety. Modern machines deliver remarkably low radiation doses—approximately one-tenth the amount of a standard chest x-ray during typical procedures. Additionally, the entire scanning process typically requires only five to ten minutes, making it convenient for busy patients.
Primary Medical Applications and Diagnostic Uses
Healthcare providers primarily order these scans to diagnose osteoporosis, a condition where bones become weak and susceptible to fractures. Similarly, doctors use these measurements to monitor bone loss in patients with various conditions affecting skeletal health significantly. Postmenopausal women represent the largest group undergoing regular screenings because hormonal changes accelerate bone density loss during this life stage.
Beyond osteoporosis detection, physicians utilize this technology to assess fracture risk in elderly patients prone to dangerous falls. In addition, endocrinologists order these tests for patients with thyroid disorders, diabetes, or other metabolic conditions affecting bone metabolism. Rheumatologists frequently request scans for patients taking corticosteroids or other medications known to compromise bone strength over extended periods.
Pediatric specialists sometimes employ this imaging technique to evaluate bone development in children with growth disorders or nutritional deficiencies. Furthermore, oncologists monitor bone health in cancer patients receiving chemotherapy or radiation treatments that potentially damage skeletal structures. The versatility of this diagnostic tool makes it invaluable across numerous medical specialties for comprehensive patient care.
Body Composition Analysis for Fitness and Health Optimization
Athletes and fitness professionals increasingly recognize the value of detailed body composition measurements beyond simple weight tracking methods. Consequently, many training facilities now offer these scans to help clients optimize their nutrition and exercise programs effectively. The technology precisely measures fat mass, lean muscle mass, and bone mineral content in different body regions accurately.
Traditional methods like bioelectrical impedance scales provide estimates that vary significantly based on hydration levels and other temporary factors. In contrast, this scanning technology delivers consistent, reproducible measurements that remain unaffected by water intake or recent meals consumed. Therefore, fitness enthusiasts can track genuine changes in muscle development and fat loss over time with remarkable confidence.
Nutritionists use detailed body composition reports to design personalized meal plans targeting specific health and performance goals effectively. Similarly, personal trainers adjust workout routines based on objective data showing muscle imbalances or areas requiring targeted development. The regional analysis feature proves particularly valuable for identifying asymmetries that might contribute to injury risk in competitive athletes.
Understanding Your Scan Results and T-Scores Explained
Medical professionals interpret bone density results using standardized scoring systems that compare individual measurements against healthy reference populations. The T-score represents the most important number on diagnostic reports, indicating how your bone density compares to healthy adults. Specifically, this score shows the number of standard deviations your measurement falls above or below the average peak bone mass.
A T-score of -1.0 or above indicates normal bone density, suggesting no significant concern regarding fracture risk currently. Meanwhile, scores between -1.0 and -2.5 indicate osteopenia, a condition representing moderately reduced bone density requiring monitoring and intervention. Ultimately, T-scores of -2.5 or lower confirm osteoporosis diagnosis, signaling substantially increased fracture risk requiring immediate medical attention.
Doctors also review Z-scores, which compare your results against age-matched peers rather than young healthy adults exclusively. These comparisons help identify whether bone loss exceeds expected age-related decline or suggests underlying medical conditions requiring investigation. Additionally, physicians track changes in bone density over time to evaluate treatment effectiveness and disease progression accurately.
Who Should Get Regular Bone Density Screenings
Medical guidelines recommend routine screenings for women aged 65 and older and men aged 70 and older regularly. However, younger individuals with specific risk factors should consider earlier testing to establish baseline measurements and detect problems. Women going through early menopause or surgical menopause particularly benefit from proactive screening to monitor accelerated bone loss.
People with family histories of osteoporosis or hip fractures face elevated risks and should discuss appropriate screening schedules. Furthermore, individuals with eating disorders, celiac disease, or inflammatory bowel disease often experience compromised nutrient absorption affecting bone health. Patients taking medications like corticosteroids, anticonvulsants, or proton pump inhibitors for extended periods require regular monitoring appointments.
Smokers and people who consume excessive alcohol face higher osteoporosis risks and should consider earlier screening than typically recommended. Additionally, individuals with thyroid disorders, rheumatoid arthritis, or chronic kidney disease benefit from proactive bone health assessments. Sedentary lifestyles and low body weight also increase fracture risks, warranting discussions with healthcare providers about appropriate testing.
The Scanning Procedure: What to Expect During Your Appointment
Patients appreciate that this diagnostic procedure requires no special preparation, injections, or invasive techniques causing discomfort or anxiety. Nevertheless, you should wear comfortable, loose-fitting clothing without metal zippers, buttons, or accessories that might interfere with imaging. Most facilities provide gowns if your clothing contains metal components that could compromise image quality during the scan.
The technologist will ask you to lie flat on a padded table while the scanning arm passes slowly overhead. Importantly, you must remain completely still during the scanning process to ensure accurate measurements and prevent motion artifacts. The machine produces no loud noises or confined spaces, making it suitable for patients with claustrophobia concerns.
Central scans examining the spine and hip typically take approximately five to ten minutes from start to finish. Meanwhile, whole-body composition scans require slightly longer scanning times to capture detailed measurements across all body regions. Afterward, you can immediately resume normal activities without any recovery period or activity restrictions following the procedure.
Preparing for Your Scan and Pre-Appointment Guidelines
Generally, this procedure requires minimal preparation compared to other medical imaging tests requiring fasting or medication adjustments beforehand. However, you should avoid taking calcium supplements for at least 24 hours before your scheduled appointment time. Calcium supplements can interfere with absorption measurements and potentially affect the accuracy of diagnostic results obtained during scanning.
Women should inform technologists if they might be pregnant, as even minimal radiation exposure warrants precautions during pregnancy. Additionally, patients should mention recent barium studies or nuclear medicine scans, which might necessitate postponing the appointment temporarily. These substances remain in the body for several days and can significantly interfere with accurate bone density measurements.
Patients should inform healthcare providers about recent fractures, surgical hardware, or joint replacements that might affect specific measurement sites. Subsequently, technologists can adjust scanning protocols or choose alternative measurement sites to obtain valid diagnostic information despite these limitations. Bringing previous scan reports helps radiologists compare current results against historical data to track changes over time accurately.
Interpreting Body Composition Reports and Regional Analysis
Body composition reports provide detailed breakdowns of fat mass, lean mass, and bone mass distributed throughout different body regions. Consequently, users can identify specific areas where they carry excess fat or lack adequate muscle development for balanced physiques. The reports typically divide the body into arms, legs, trunk, and total body measurements for comprehensive analysis.
Android fat refers to abdominal fat accumulation, which carries higher health risks compared to gynoid fat distributed in hips. Therefore, tracking changes in android-to-gynoid ratios helps assess cardiovascular disease risk and metabolic syndrome progression over time. Many reports also calculate visceral adipose tissue estimates, indicating dangerous fat surrounding internal organs within the abdominal cavity.
Muscle mass symmetry measurements help identify imbalances between left and right sides that might increase injury risk during athletic activities. Similarly, athletes can track changes in specific muscle groups to evaluate training program effectiveness and adjust exercise protocols accordingly. The detailed regional data proves invaluable for rehabilitation specialists working with patients recovering from injuries or surgical procedures.
Cost Considerations and Insurance Coverage Information
The cost of bone density testing varies considerably depending on geographic location, facility type, and insurance coverage available. Typically, medical centers charge between $125 and $350 for standard diagnostic scans ordered by physicians for medical purposes. However, body composition scans marketed toward athletes and fitness enthusiasts often cost less, ranging from $75 to $150 per session.
Medicare covers bone density testing for eligible beneficiaries meeting specific criteria every two years under preventive care benefits. Most private insurance plans also cover medically necessary scans for patients with documented risk factors or clinical indications. Nevertheless, insurance companies typically do not cover body composition scans requested solely for fitness tracking or athletic performance purposes.
Patients should verify coverage details with insurance providers before scheduling appointments to avoid unexpected out-of-pocket expenses after procedures. Some facilities offer package deals for individuals wanting regular body composition monitoring without insurance coverage for these optional services. Additionally, health savings accounts and flexible spending accounts can often cover these costs as qualified medical expenses.
Radiation Exposure and Safety Considerations
Many patients express concerns about radiation exposure from medical imaging procedures, but these scans involve minimal radiation doses. Specifically, the effective radiation dose typically measures less than 0.001 millisieverts for standard spine and hip examinations. Comparatively, this represents a tiny fraction of natural background radiation people receive annually from environmental sources like cosmic rays.
The radiation dose from one scan equals approximately one-tenth of a standard chest x-ray or one day of natural background radiation. Therefore, medical experts consider the diagnostic benefits far outweigh the negligible risks associated with this minimal radiation exposure. Modern equipment incorporates advanced shielding and collimation technology that focuses radiation precisely on measurement sites only.
Pregnant women should avoid unnecessary radiation exposure, though the minimal doses involved pose relatively low risks to developing fetuses. Nevertheless, physicians typically postpone non-urgent scans until after delivery to eliminate any potential concerns about fetal exposure. Nursing mothers can safely undergo these procedures without needing to pump and discard breast milk afterward.
Comparing Alternative Bone Density Measurement Methods
Several alternative technologies exist for assessing bone density, though most lack the precision and reliability of dual-energy x-ray systems. Quantitative computed tomography provides three-dimensional bone density measurements but delivers significantly higher radiation doses to patients. Consequently, physicians reserve this technology for specific situations where standard scanning proves inadequate for diagnostic purposes.
Ultrasound densitometry offers a radiation-free alternative that measures bone properties in peripheral sites like the heel or forearm. However, these measurements cannot directly assess critical sites like the spine and hip where fractures cause the most serious complications. Therefore, ultrasound screening serves primarily as an initial assessment tool requiring confirmation with more definitive testing methods.
Quantitative ultrasound devices provide convenient screening in community settings like health fairs or pharmacy wellness programs for public outreach. Nevertheless, abnormal ultrasound results always require follow-up with standard scanning for definitive diagnosis and treatment planning purposes. Medical professionals do not consider peripheral measurements adequate for monitoring treatment effectiveness or tracking disease progression over time.
Tracking Progress and Follow-Up Scanning Schedules
Physicians typically recommend follow-up scans every one to two years for patients diagnosed with osteopenia or osteoporosis undergoing treatment. Meanwhile, individuals with normal bone density may not require repeat testing for several years unless new risk factors develop. Treatment decisions depend significantly on whether bone density remains stable, improves, or continues declining despite therapeutic interventions.
Athletes and fitness enthusiasts using body composition tracking often schedule scans every three to six months to monitor training progress. However, more frequent scanning provides little additional benefit because significant body composition changes require several months to manifest measurably. Therefore, quarterly scans typically provide optimal frequency for tracking meaningful changes without unnecessary expense or radiation exposure.
Consistent measurement conditions improve the reliability of serial comparisons by minimizing technical variations unrelated to actual biological changes. Consequently, patients should return to the same facility using the same equipment model when possible for follow-up examinations. Technologists should also position patients identically to ensure measurements capture the exact same skeletal regions across all scanning sessions.
Lifestyle Factors Affecting Bone Density and Body Composition
Nutrition plays a crucial role in maintaining healthy bones, with calcium and vitamin D representing the most critical nutrients. Adults should consume 1,000 to 1,200 milligrams of calcium daily through dietary sources or supplements as recommended by physicians. Similarly, adequate vitamin D levels ensure proper calcium absorption, requiring supplementation for many individuals lacking sufficient sun exposure.
Weight-bearing exercises like walking, jogging, and resistance training stimulate bone formation and help maintain or increase bone density. In contrast, sedentary lifestyles accelerate bone loss and increase fracture risks as people age without adequate physical activity. Athletes must balance intense training with adequate recovery periods to avoid stress fractures from excessive mechanical loading patterns.
Smoking cessation represents one of the most important interventions for improving bone health and reducing fracture risk significantly. Likewise, limiting alcohol consumption to moderate levels helps preserve bone density and prevent accelerated skeletal deterioration over time. Maintaining healthy body weight prevents excessive mechanical stress on bones while ensuring adequate hormonal support for bone metabolism.
Medical Treatments and Interventions Based on Results
Physicians prescribe various medications to slow bone loss or stimulate new bone formation depending on disease severity and patient characteristics. Bisphosphonates represent the most commonly prescribed drugs, working by inhibiting cells that break down bone tissue during normal remodeling. These medications can reduce fracture risk by 40 to 70 percent in patients with established osteoporosis when taken consistently.
Selective estrogen receptor modulators provide an alternative for postmenopausal women who cannot tolerate bisphosphonates or prefer different mechanisms. Meanwhile, denosumab injections offer convenient twice-yearly dosing for patients with difficulty adhering to oral medication schedules requiring specific timing. Anabolic agents like teriparatide actually stimulate new bone formation rather than merely preventing loss in severe cases.
Hormone replacement therapy may benefit some postmenopausal women, though doctors carefully weigh cardiovascular and cancer risks against skeletal benefits. Additionally, treating underlying conditions contributing to bone loss often proves essential for achieving optimal treatment outcomes with medications. Regular monitoring with follow-up scans helps physicians adjust treatment plans based on individual patient responses to therapeutic interventions.
Special Considerations for Athletes and Active Individuals
Competitive athletes often develop very low body fat percentages that can compromise bone health despite high activity levels. Female athletes face particular risks when low energy availability disrupts normal menstrual function, leading to accelerated bone loss. Consequently, sports medicine physicians monitor bone density carefully in athletes showing signs of relative energy deficiency in sport.
Body composition tracking helps athletes optimize their physiques for sport-specific performance requirements without compromising overall health or recovery. For instance, endurance athletes may prioritize minimizing excess weight while maintaining adequate muscle mass for power generation. Strength athletes focus on maximizing muscle development while keeping body fat within healthy ranges supporting optimal hormonal function.
Recovery from injuries or surgeries benefits from objective tracking of muscle loss and regain during rehabilitation periods away from training. Subsequently, athletic trainers can design evidence-based return-to-sport protocols ensuring athletes regain adequate strength before resuming full competition schedules. The detailed regional analysis helps identify lingering deficits requiring targeted intervention before clearing athletes for unrestricted participation.
Future Developments and Emerging Technologies
Researchers continue refining scanning technology to provide even more detailed body composition analysis with improved accuracy and reduced costs. Artificial intelligence algorithms now help interpret complex scan data, identifying subtle patterns that might indicate early disease or suboptimal health. These advances promise to make comprehensive body composition analysis more accessible to broader populations for preventive health management.
Three-dimensional imaging capabilities under development will provide unprecedented visualization of bone architecture beyond simple density measurements alone. Consequently, physicians will better predict fracture risk by assessing bone quality and microstructure in addition to mineral content. These technological improvements may revolutionize osteoporosis diagnosis and treatment monitoring in coming years significantly.
Portable scanning devices currently in development could bring this diagnostic capability to remote areas lacking access to major medical centers. Furthermore, reduced equipment costs may enable more physicians to offer in-office scanning, improving convenience and potentially increasing screening rates. These innovations promise to democratize access to advanced body composition analysis for diverse populations worldwide seeking optimal health.
Final Remarks: Empowering Health Through Advanced Diagnostic Technology
This remarkable imaging technology provides invaluable insights into skeletal health and body composition that empower individuals to make informed decisions. Medical professionals rely on accurate bone density measurements to diagnose osteoporosis early and implement treatments preventing devastating fractures. Athletes and fitness enthusiasts benefit from objective data guiding their training programs toward optimal performance and physique development goals.
Regular screening for appropriate populations enables early detection of bone loss when interventions prove most effective for preventing complications. The minimal radiation exposure and quick, non-invasive procedure make this diagnostic tool ideal for routine monitoring without significant burden. Consequently, more people should discuss screening options with healthcare providers to take proactive control of their skeletal health.
Understanding scan results and their implications helps patients participate actively in treatment decisions and lifestyle modifications affecting long-term outcomes. The comprehensive body composition data available through modern scanning technology extends far beyond simple bone density measurements originally intended. Ultimately, this advanced diagnostic capability represents a powerful tool for optimizing health, preventing disease, and achieving personal wellness goals.